November 2025
Gastrointestinal Health and Infection Diagnostic Solutions
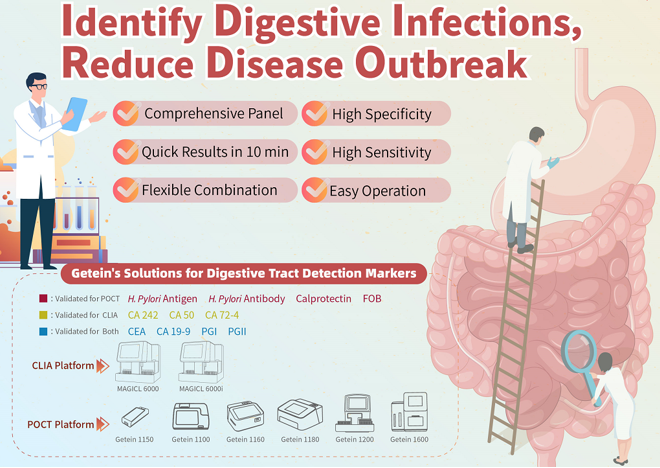
Gastrointestinal health is a critical factor influencing overall human well-being. Digestive diseases such as Inflammatory Bowel Disease (IBD), Colorectal Cancer (CRC), and Helicobacter pylori infection, if not diagnosed and managed promptly, can significantly impact patients' quality of life. Statistics indicate that colorectal cancer is the third most common cancer globally, while H. pylori infection affects approximately half of the world's population.

Diagnostic Biomarkers for Gastrointestinal Inflammation and Infection
Modern diagnostic medicine utilizes specific biomarkers to provide accurate, non-invasive testing solutions for gastrointestinal inflammatory and infectious diseases. These biomarkers facilitate early screening, disease activity assessment, and treatment efficacy monitoring.
Detailed Overview of Core Diagnostic Biomarkers
Calprotectin
Calprotectin is a key protein complex abundant in neutrophils, serving as a highly sensitive and specific biomarker for assessing intestinal inflammation.
Clinical Applications:
Guideline-recommended marker for screening Inflammatory Bowel Disease (IBD)
Evaluating IBD activity for optimized disease management
An indicator for certain inflammatory conditions
Fecal Occult Blood Test (FOBT)
The Fecal Occult Blood Test is a simple, non-invasive diagnostic tool designed to detect hidden (occult) blood in stool samples—blood not visible to the naked eye—which often indicates underlying gastrointestinal abnormalities.
Clinical Applications:
Early-stage Colorectal Cancer (CRC) screening
Evaluating gastrointestinal bleeding of unknown origin
Routine examination for gastrointestinal disorders
Helicobacter pylori Detection
H. pylori Antigen Test
This test identifies specific bacterial antigens in stool samples, making it ideal for detecting active infections.
H. pylori Antibody Test
This test detects antibodies (IgG, IgM, IgA) produced by the immune system in response to past or present H. pylori exposure, providing historical infection data.
Clinical Applications:
Aiding in the diagnosis of H. pylori-related disorders
Guiding antibiotic treatment decisions
Monitoring post-therapy eradication success
Clinical Application Guidelines
|
Test Parameter |
Primary Use |
Application Scenarios |
|
Calprotectin |
Intestinal inflammation assessment |
IBD screening and monitoring, inflammatory disease differentiation |
|
Fecal Occult Blood |
GI bleeding screening |
Early CRC screening, GI bleeding localization |
|
H. pylori Antigen |
Active infection diagnosis |
Dyspepsia etiology investigation, pre-treatment evaluation |
|
H. pylori Antibody |
Infection history assessment |
Epidemiological studies, immune response monitoring |
Reference
1. Gismera CS, Aladrén BS. Inflammatory bowel diseases: a disease (s) of modern times? Is incidence still increasing? World J Gastroenterol. 2008;14:5491–8.
2. Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54. e42. quiz e30.
3. World Gastroenterology Organisation. Inflammatory Bowel Disease. WGO; 2015. [Accessed 18 September 2018]. World Gastroenterology Organisation Global Guidelines. http://www.worldgastroenterology.org/UserFiles/file/guidelines/inflammatory-bowel-disease-english-2015-update.pdf. [Google Scholar]
4. IBD Working Group of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. Inflammatory bowel disease in children and adolescents: recommendations for diagnosis–the Porto criteria. J Pediatr Gastroenterol Nutr. 2005;41:1–7.
5. Stange EF, Travis SP, Vermeire S, Beglinger C, Kupcinkas L, Geboes K, et al. European Crohn’s and Colitis Organisation. European evidence based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. Gut. 2006;55(Suppl 1):i1–15.
6. Van Rheenen PF, Van de Vijver E, Fidler V. Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis. BMJ. 2010;341:c3369.
7. Menees SB, Powell C, Kurlander J, Goel A, Chey WD. A meta-analysis of the utility of C-reactive protein, erythrocyte sedimentation rate, fecal calprotectin, and fecal lactoferrin to exclude inflammatory bowel disease in adults with IBS. Am J Gastroenterol. 2015;110:444–54.
8. Bernstein CN, Fried M, Krabshuis JH, Cohen H, Eliakim R, Fedail S, et al. World Gastroenterology Organization Practice Guidelines for the diagnosis and management of IBD in 2010. Inflamm Bowel Dis. 2010;16:112–24.
9. Diamanti A, Panetta F, Basso MS, Forgione A, Colistro F, Bracci F, et al. Diagnostic work-up of inflammatory bowel disease in children: the role of calprotectin assay. Inflamm Bowel Dis. 2010;16:1926–30.
10. Dignass A, Eliakim R, Magro F, Maaser C, Chowers Y, Geboes K, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012;6:965–90.
11. Van Assche G, Dignass A, Reinisch W, van der Woude CJ, Sturm A, De Vos M, et al. European Crohn’s and Colitis Organisation (ECCO) The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Special situations. J Crohns Colitis. 2010;4:63–101.
12. Von Roon AC, Karamountzos L, Purkayastha S, Reese GE, Darzi AW, Teare JP, et al. Diagnostic precision of fecal calprotectin for inflammatory bowel disease and colorectal malignancy. Am J Gastroenterol. 2007;102:803–13.
13. Moniuszko A, Głuszek S, Rydzewska G. Rapid fecal calprotectin test for prediction of mucosal inflammation in ulcerative colitis and Crohn disease: a prospective cohort study. Pol Arch Intern Med. 2017;127:312–8.
14. Henderson P, Anderson NH, Wilson DC. The diagnostic accuracy of fecal calprotectin during the investigation of suspected pediatric inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol. 2014;109:637–45.

Open WeChat and Scan the QR Code. Stay Tuned with Us.