January 2023

COVID-19 caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was officially declared a pandemic by the World Health Organization in March 2020[1,3] . According to European Centre for Disease Prevention and Control, the rate of COVID-19 cases among people aged 65 years and older increased by 7% by the week ending 18 December 2022 compared with the previous week, reaching 43% of the maximum value reported during the pandemic[12].

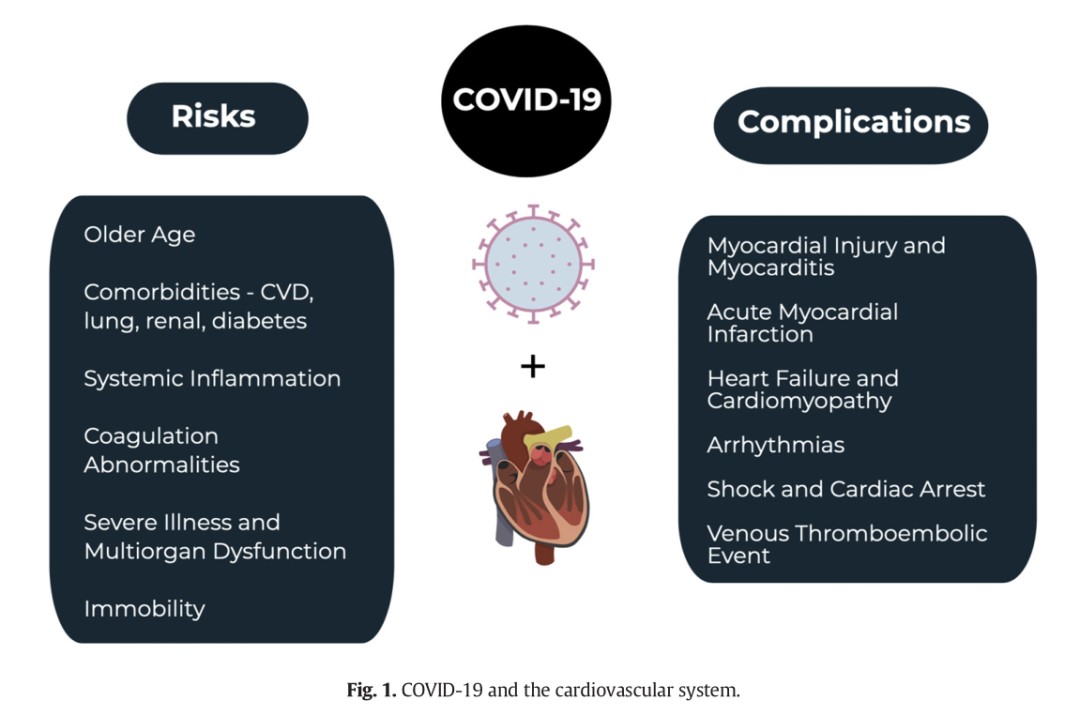
COVID-19 is associated with a number of complications, including fatigue, pulmonary problems, cognitive dysfunction and cardiovascular issues such as myocardial injury and myocarditis, AMI, heart failure, dysrhythmias, and VTE. While much of the focus has been on the pulmonary complications, it is important for emergency clinicians to be aware of the cardiovascular complications, which can be as significant contributor to the mortality associated with this disease[4-9]. A meta-analysis of 1527 patients with COVID-19 found that the prevalence of hypertension was 17.1% and cardiac disease was 16.4%, and that these patients were more likely to require critical care[10]. Another study of 44,672 patients with COVID-19 found that a history of CVD was associated with a nearly five-fold increase in the case fatality rate when compared with patients without CVD (10.5% vs. 2.3%)[5]. Other studies suggest similar findings with increased risk of mortality in patients with prior CVD[5-9,11].
Myocardial injury and myocarditis associated with COVID-19
One of the first reports of myocardial injury associated with SARS-CoV-2 showed that there were 12% of patients had a high-sensitivity troponin I above the threshold of 28 pg/mL[7]. Subsequent studies have found that myocardial injury with an elevated troponin level may occur in 7–17% of patients hospitalized with COVID-19 and 22–31% of those admitted to the intensive care unit (ICU)[7-9]. Myocarditis has also been identified with high viral loads and mononuclear infiltrates identified on autopsy of some patients with COVID-19[13-15]. In fact, one study suggested that up to 7% of COVID-19 related deaths were due to myocarditis[6].
Acute myocarditis presents across a variable range of clinical severity and is a significant diagnostic challenge in the COVID-19 era. Patients with COVID-19 can present with chest pain, dyspnea, dysrhythmia, and acute left ventricular dysfunction[5-9]. Inpatients with myocarditis and myocardial injury, serum troponin values will be abnormal.
Therefore, early recognition of any early warning signs of cardiovascular complications caused by COVID-19 and timely access to appropriate clinical management are critical elements of care to reduce the risk of severe cardiovascular complications and death due to COVID-19.
Myocardial injury and myocarditis associated with COVID-19
One of the first reports of myocardial injury associated with SARS-CoV-2 showed that there were 12% of patients had a high-sensitivity troponin I above the threshold of 28 pg/mL[7]. Subsequent studies have found that myocardial injury with an elevated troponin level may occur in 7–17% of patients hospitalized with COVID-19 and 22–31% of those admitted to the intensive care unit (ICU)[7-9]. Myocarditis has also been identified with high viral loads and mononuclear infiltrates identified on autopsy of some patients with COVID-19[13-15]. In fact, one study suggested that up to 7% of COVID-19 related deaths were due to myocarditis[6].
Acute myocarditis presents across a variable range of clinical severity and is a significant diagnostic challenge in the COVID-19 era. Patients with COVID-19 can present with chest pain, dyspnea, dysrhythmia, and acute left ventricular dysfunction[5-9]. Inpatients with myocarditis and myocardial injury, serum troponin values will be abnormal.
Therefore, early recognition of any early warning signs of cardiovascular complications caused by COVID-19 and timely access to appropriate clinical management are critical elements of care to reduce the risk of severe cardiovascular complications and death due to COVID-19.
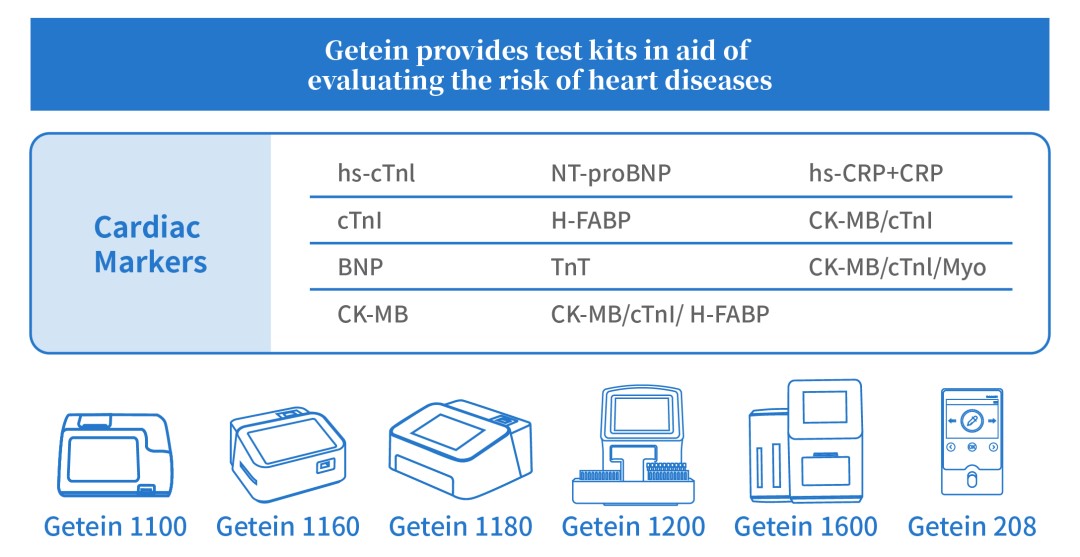
Getein will continuously pay close attention to global health issues and needs in real time, to help recognize cardiovascular complications caused by COVID-19, reduce the burden on healthcare systems and optimize patient management.
References:
[1] World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020.
[2] Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention.
[3] World Health Organization. Situation report.
[4] Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients,
health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol Mar 18 2020 [pii: S0735-1097(20)34637-4, in press].
[5] Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus
disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA Feb 24 2020.
[6] Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China.
[7] Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506.
[8] Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet Mar 28
2020;395(10229):1054–62.
[9] Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA Feb 7 2020.
[10] Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol Mar 11 2020.
[11] Murthy S, Gomersall CD, Fowler RA. Care for critically ill patients with COVID-19. JAMA Mar 11 2020.
[12] Country overview report: week 50 2022. European Centre for Disease Prevention and Control.
[13] Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) Feb 7 2020.
[14] Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med Apr 2020;8(4):420–2.
[15] Liu Y, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci 2020;63:
364–74.

Open WeChat and Scan the QR Code. Stay Tuned with Us.